Haemorrhoids
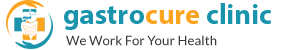
 Hemorrhoids or piles as are commonly called are actually enlarged vascular cushions normally present in the anal canal. Depending on their position they are either external or internal piles. Depending on the extent of enlargement, they are classified from grades 1 to 4. Constipation and excessive straining for passing stools is the single most important reason for enlargement of hemorrhoids.
Hemorrhoids or piles as are commonly called are actually enlarged vascular cushions normally present in the anal canal. Depending on their position they are either external or internal piles. Depending on the extent of enlargement, they are classified from grades 1 to 4. Constipation and excessive straining for passing stools is the single most important reason for enlargement of hemorrhoids.
Patients usually present with pain while passing stools, bleeding and swellings around the anus. Bleeding is usually fresh blood which occurs at the end of motion. Bleeding can be so mild and can present as anemia or can be severe enough to need transfusions. Grades 1 and 2 hemorrhoids are usually not visible outside but present with bleeding or pain. Grade 3 and 4 hemorrhoids are when they prolapse out.
Diagnosis is done by clinical examination and a flexible sigmoidoscopy. Since everyone has hemorrhoids, a very important aspect of treatment of hemorrhoids involves excluding other causes like cancers and colitis.
Majority of patients usually delay in approaching treatment due to the inherent social stigma and fear of painful treatments. Safe and painless treatment options are available presently and patients no more need to suffer unnecessarily. Current principles of treatment rely on shrinking the size of the hemorrhoids and not disturbing the sensitive skin around the anal canal. This ensures long lasting effective cure and also preservation of normal sensation and control of stools. Treatment depends on the extent of the patient’s symptoms, medical problems faced by the patients and the grade of hemorrhoids.
Medical treatment: Small (Grade 1 or2) with mild symptoms can be treated with medications. Treatment involves stool softeners preferably fiber based and flavonoids. This is the first line of treatment either alone or in combination of other procedures as described below.
Laser Haemorrhoidoplasty: Grade 3 hemorrhoids or patients with bleeding can benefit from laser haemorrhoidoplasty. LASER energy ablates the hemorrhoidal vascular plexus leading to stoppage of bleeding and shrinking of hemorrhoids. Since there is no cutting involved, pain is less and this can be performed as a day care procedure.
Stapler Haemorrhoidectomy/pexy: Prolapsed and grade 4 hemorrhoids are best treated with a stapler or conventional haemorrhoidectomy. Here the hemorrhoidal pedicles are excised above the dentate line. Since the sensitive skin area is not cut postoperative pain is minimal.
Fissure in ano
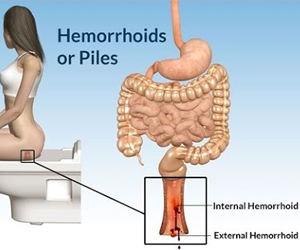
 This is a painful condition arising from an acute tear in the anal canal mainly due to constipation. Majority of people present with severe pain and bleeding occasionally while passing stools. All the patients usually associate the symptoms with passing hard stools. Fissure can be of two types which include
This is a painful condition arising from an acute tear in the anal canal mainly due to constipation. Majority of people present with severe pain and bleeding occasionally while passing stools. All the patients usually associate the symptoms with passing hard stools. Fissure can be of two types which include
Acute Fissure: Excessive stretch of the anal canal due to straining while passing stools results in the tear exposing the underlying nerves and blood vessels. This leads to spasm of the underlying sphincter and causes the excruciating pain.
Recurrent Fissure: Some patients have excessively tight anal opening leading to repeated episodes of fissure.
Chronic Fissure: Patients with long standing fissure or diseases like tuberculosis or Crohn’s disease have non healing fissure. These patients have long standing dull pain and bleeding.
Treatment options depend on the severity and duration of symptoms. The main principle is relieving the sphincter spasm and/or removal of scarred skin.
Medical Treatment: This is the initial treatment in majority and the only treatment needed in two thirds of patients. This comprises of stool softeners and topical creams with muscle relaxants. Patients usually need a week or two of treatment for effective cure.
Laser/ lateral Sphincterotomy: Surgery is offered in patients who either fail medical therapy or have repeated recurrences following treatment. Lateral sphincterotomy is usually performed as a day care procedure and does not need hospitalisation. Use of Laser reduces pain.
Botox Injections: This can offered in bedridden patients or for those who have long standing inflammatory conditions of anal canal where surgery is better avoided. The drawback involves patients tend to have a temporary control of pain.
Fistula
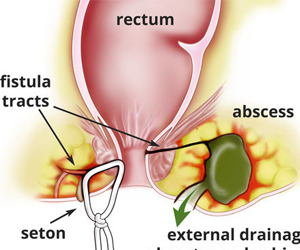 Fistula is an abnormal communication from the anal canal to the external skin. Because of this patients usually suffer from pain and pus discharge from near the anal canal. Sometimes patients present with swelling and severe pain when they develop pus collection called as perianal abscess.
Fistula is an abnormal communication from the anal canal to the external skin. Because of this patients usually suffer from pain and pus discharge from near the anal canal. Sometimes patients present with swelling and severe pain when they develop pus collection called as perianal abscess.
Based on the location of the internal opening to the anal canal and the relation of the fistula track to the surrounding muscles, they are classified as either or low or high anal fistulae. Majority of the fistulas result from constipation and bacterial infections. Some chronic diseases like tuberculosis or Crohn’s disease can also lead to secondary fistulas.
Evaluation of the patients include
- flexible sigmoidoscopy/ colonoscopy to evaluate the intestine
- ultrasound or MRI perineum with fistulogram for delineating the extent and course of the fistula tracts
No two patients have a similar track and hence treatment needs to be individualized. All fistulae, unless secondary to Crohn’s disease or tuberculosis, need some surgical intervention for definitive cure. The key principles of treatment include
- closing the internal opening and
- safe ablation of the track without damaging the sphincter muscles
These can be achieved with various techniques like
- Fistulotomy: Involves laying open the tract for it to heal. This is the simplest technique and used in small fistulas
- Fistulectomy: This involves removal of the tract either by conventionally or by minimal access using FIXcision.
- Laser Ablation: Involves burning of the tracts by a radial LASER fiber. useful in complex high fistulae. helps in faster healing
- LIFT, Mucosal plug, Endoanal flap: for complex high fistulas
The ideal technique depends on the individual patients and his clinical condition and involves a combination of above methods. Loss of control on stools and possibility of recurrence are among the most common concerns for the patients prior to surgery. While continence can always be preserved by meticulous planning and execution of surgery, recurrence rates can be reduced with proper follow up dressings ensuring satisfactory healing. Recent advances in laser help in reducing the wounds and need for postoperative dressings. Treatment of secondary fistulas depends on the primary disease.
Rectal Prolapse
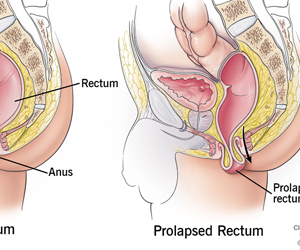 This is the condition in which the last portion of the rectum and anal canal protrude through the anal opening due to loosening of the posterior fixation to the sacrum. Patients present with inability to evacuate stools often needing manual evacuation. Some complain of swelling while passing stools and occasionally bleeding. This condition is often undiagnosed since the prolapse occurs only during passing stools and is not visible on cursory examination. Sometimes this condition is often confused with haemorrhoids leading to suboptimal treatment.
This is the condition in which the last portion of the rectum and anal canal protrude through the anal opening due to loosening of the posterior fixation to the sacrum. Patients present with inability to evacuate stools often needing manual evacuation. Some complain of swelling while passing stools and occasionally bleeding. This condition is often undiagnosed since the prolapse occurs only during passing stools and is not visible on cursory examination. Sometimes this condition is often confused with haemorrhoids leading to suboptimal treatment.
Important consideration in the diagnosis involves a colonoscopy to exclude colonic tumors. MRI defaecogram helps in assessing the perineal musculature and the extent of prolapse. Treatment involves
- strengthening of the perineal muscles to reduce the amount of prolapse and
- relieving constipation by stool softeners
Perineal exercises alone help in relieving symptoms in patients with small prolapse. Patients with large rectal prolapse are better treated with transabdominal approach, rectopexy which involves fixing the redundant rectum to lower part of backbone. This can either be done by suturing or with reinforcement with a mesh for better long term results. Patients with large prolapse or with severe constipation do better with the removal of the redundant rectum along with fixation (resection rectopexy). Both these can be performed laparoscopically for enhanced recovery.
Diverticulosis
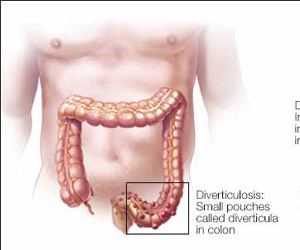 This is the condition in which small out-pouchings develop in the large intestine due to excessive pressure within the intestine. Colonic diverticulae can broadly be classified as right sided or left sided, the left sided ones being more common.
This is the condition in which small out-pouchings develop in the large intestine due to excessive pressure within the intestine. Colonic diverticulae can broadly be classified as right sided or left sided, the left sided ones being more common.
Right Colonic Diverticulae: These affect the right sided colon. Since these are right sided, pain is usually on the right side of the abdomen and often confused with appendicitis. However, their more common complication is bleeding which needs either colonoscopy or surgery.
Left Colonic Diverticulae: These are more common and are the result of prolonged constipation and excessive straining by the patients. They mainly affect the sigmoid colon. The disease severity can vary from mild pain and constipation associated with diverticulosis (presence of diverticulae) to symptoms of sepsis when they get infected (diverticulitis). Bacteria along with faecal matter tend to accumulate in these outpouchings and cause serious infections. When untreated initially, they can ultimately lead to life threatening acute abdomen (complicated diverticulitis/ perforation). Repeated episodes of infection over a period of time lead to scarring and narrowing of the intestine called as colonic stricture, which presents as intestinal obstruction. These patients are also more prone to colonic tumors.
Treatment is based on the general condition of the patient and severity of the disease. Stool softeners and antibiotics are adequate for mild disease while surgery is needed in severe disease. Surgery is complicated in view of sepsis and feces laden colon. The main principle of the treatment involves removal of the affected colon and clearing the infected focus. This can either be done as a single stage procedure when patients’ condition is stable. However in presence of severe sepsis, it is preferable to split the surgery into a two stage procedure for patient safety. However with recent advances, laparoscopic surgery and single stage procedures can be offered to patients who present early for treatment.
These conditions include irritable bowel syndrome, constipation, hemorrhoids, anal fissures, abscess, colitis, polyps and colon cancer.