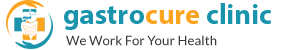
Pancreatic Cancers
 Pancreatic tumors present problems in diagnosis and treatment due to their deep location and relation to important blood vessels. Grossly pancreatic tumors are of three types
Pancreatic tumors present problems in diagnosis and treatment due to their deep location and relation to important blood vessels. Grossly pancreatic tumors are of three types
- Ductal tumors: Majority of tumors arising in pancreas originate from the ductal tissue (ductal adenocarcinoma). These are very aggressive tumours and early diagnosis is important for a good outcome.
- Cystic tumors: These are more commonly seen in younger patients. They usually grow rapidly and present as large tumors. However since they tend to remain localized to pancreas, surgery offers lasting cure in these patients.
- Rare tumors: Tumors like IPMN are rare but now being increaingly detected on screening.
Pancreas being a deep seated organ results in delayed onset of symptoms thus making screening essential for early diagnosis. The common risk factors include smoking, obesity, hereditary (BRCA 2 mutations) and chronic pancreatitis. Patients usually complain of pain radiating to back, jaundice, vomiting and unexplained weight loss. Worsening of diabetes in chronic pancreatitis is also an early sign.
Diagnosis is usually established after a contrast enhanced CT scan or ERCP. Treatment and outcome exclusively depend on the stage of the tumor. Patients with early tumors benefit with pancreatectomy followed by chemotherapy. Patients with advanced tumors usually are very sick and only palliative care is offered.
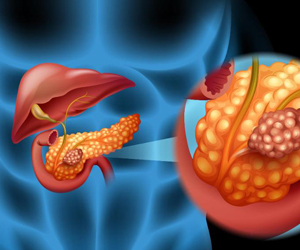
Acute Pancreatitis
 Patients usually present with excruciating pain and severe metabolic abnormalities. Some patients who have severe pancreatitis present with features of sepsis, kidney/ respiratory failure.Most common causes for pancreatitis include
Patients usually present with excruciating pain and severe metabolic abnormalities. Some patients who have severe pancreatitis present with features of sepsis, kidney/ respiratory failure.Most common causes for pancreatitis include
- Alcohol
- Gallstones
- Herreditary/ genetic causes
- Rare conditions like hypercalcemia and high triglycerides
This is the condition associated with activation of pancreatic digestive enzymes outside the gastrointestinal tract. The digestive enzymes meant for digesting food start dissolving and damaging normal body tissues and also enter blood stream. This leads to complications locally in the form of necrosis (devitalised tissues), perforation of intestines and bleeding from blood vessels. Systemic (generealised) complications include kidney or respiratory failure.
Initial management needs intensive ICU care aimed at correcting the abnormalities and preventing further complications. Following resuscitation and stabilisation, attention is directed at correcting the cause for pancreatitis (like gallstones) and assessing the severity of pancreatitis usually by CT scan. Infections are a serious problem in these patients and prevention is the best option. Established intraabdominal infections not responding to medical treatment may need surgical intervention for stabilization. Role of surgery includes removing devitalized infected tissue (necrosectomy) or drainage of infected fluids (abscess). In view of friable tissues due to severe inflammation and brittle condition of patients, these procedures are challenging to surgeons and critical care specialists alike. However minimal invasive methods and advances in supportive treatment help in improving the outcomes in these patients. Patients with gall stone related pancreatitis benefit from ERCP followed by laparoscopic cholecystectomy to prevent further attacks.
Chronic Pancreatitis
 Patients who have repeated attacks of pancreatitis develop pancreatic duct stones and strictures leading to continued symptoms. Long standing chronic pancreatitis is associated with permanent loss of pancreatic function and pancreatic cancers. Loss of pancreatic function is usually diagnosed when patients develop indigestion and weight loss (exocrine insufficiency) and/or diabetes (endocrine insufficiency).
Patients who have repeated attacks of pancreatitis develop pancreatic duct stones and strictures leading to continued symptoms. Long standing chronic pancreatitis is associated with permanent loss of pancreatic function and pancreatic cancers. Loss of pancreatic function is usually diagnosed when patients develop indigestion and weight loss (exocrine insufficiency) and/or diabetes (endocrine insufficiency).
Treatment is aimed at correcting the cause of pancreatitis and treatment of pancreatic insufficiency. Surgery is helpful in patients with correctable conditions like stones and strictures. Though the main aim is long term pain relief, further loss of pancreatic function can also be prevented by drainage procedures (lateral pancreaticojejunostomy). Surgery is also needed in some of these patients when there is an established or suspected tumor. Contrary to common misconception, safe and effective surgery can be performed by experienced surgeons.