We give the best Services
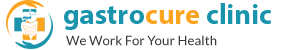
 Laparoscopic surgery are minimal access procedures in which complicated intrabdominal surgeries are done through keyholes (called as ports) without opening the abdomen. Minimally invasive surgeries involve holes9called as ports) instead of incisions for operating within the abdomen. The benefits of this include
Laparoscopic surgery are minimal access procedures in which complicated intrabdominal surgeries are done through keyholes (called as ports) without opening the abdomen. Minimally invasive surgeries involve holes9called as ports) instead of incisions for operating within the abdomen. The benefits of this include
- Reduced stress response associated with surgeries helping in safer and faster recovery
- Less postoperative pain
- Fewer complications like lung infections and cardiac problems
- Absence of wound related complications like infections, delayed healing and hernias.
Minilap ports (3mm) ports further reduce the pain and give a scarless surgery. Laparoscopic techniques can be extended to majority of the procedures previously performed as open surgeries.
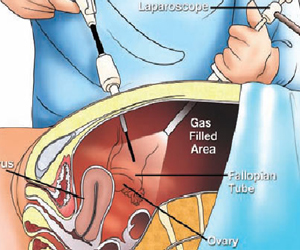
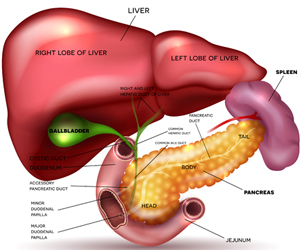
 This is the procedure performed to treat gallbladder stones which are increasingly becoming common. The principle is to safely remove the diseased gallbladder along with stones without damaging the surrounding important organs like pancreas, liver and intestine. In patients with uncomplicated stones, this can be done as a daycare procedure. Also, this can be performed with a single port (SILS) through the umbilicus for a truly scar less surgery. Contrary to general misconception, cholecystectomy does not impair digestion or increase ‘gas problems’.
This is the procedure performed to treat gallbladder stones which are increasingly becoming common. The principle is to safely remove the diseased gallbladder along with stones without damaging the surrounding important organs like pancreas, liver and intestine. In patients with uncomplicated stones, this can be done as a daycare procedure. Also, this can be performed with a single port (SILS) through the umbilicus for a truly scar less surgery. Contrary to general misconception, cholecystectomy does not impair digestion or increase ‘gas problems’.
The same procedure can also be performed in complicated stone disease like
- Acute cholecystitis: Here the infected or ruptured gall bladder is removed along with clearing any pus collections in the abdomen
- Bileduct stones: Here even the bile duct can be cleared of the slipped stones after removal of the gall bladder.
This surgery is now being performed with minilap ports, hence there is no need for any stitches or bed rest following the surgery. patients can resume normal diet and activity from the next day.
 This is the surgery aimed at treating appendicitis and its complications. The diseased appendix is safely removed along with proper drainage of pus/ inflammatory fluid. This helps in assured and safe recovery from the painful appendicitis. Current indications suggest early appendicectomy since it ensures assured recovery and prevents repeated attacks of appendicitis. Previously patients with delayed presentation including complications like inflammatory lump and pus collections were initially treated with antibiotics. Surgery was offered after a gap of 6 weeks for the inflammation to settle. However, with modern laparoscopy and supportive care, even complicated appendicitis with intrabdominal collections and appendicular lumps can be treated in the initial admission. This not only reduces hospital stay but also ensures faster recovery.
This is the surgery aimed at treating appendicitis and its complications. The diseased appendix is safely removed along with proper drainage of pus/ inflammatory fluid. This helps in assured and safe recovery from the painful appendicitis. Current indications suggest early appendicectomy since it ensures assured recovery and prevents repeated attacks of appendicitis. Previously patients with delayed presentation including complications like inflammatory lump and pus collections were initially treated with antibiotics. Surgery was offered after a gap of 6 weeks for the inflammation to settle. However, with modern laparoscopy and supportive care, even complicated appendicitis with intrabdominal collections and appendicular lumps can be treated in the initial admission. This not only reduces hospital stay but also ensures faster recovery.
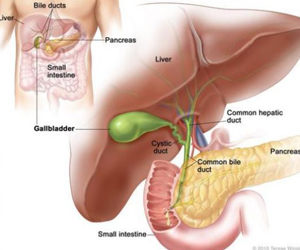
 These are the procedures in treating various abdominal hernias like incisional, inguinal or umbilical hernia. The key principles of hernia surgery include
These are the procedures in treating various abdominal hernias like incisional, inguinal or umbilical hernia. The key principles of hernia surgery include
- Safe reduction of abdominal contents to their proper location
- Tension free repair, to ensure no stress on the sutures
- Reinforcement by an adequately sized prosthetic mesh. Not only the hernia defect, all the adjacent weakened areas need to be buttressed with the mesh to reduce recurrence.
Since hernia by itself occurs due to weakened muscles, laparoscopic repairs tend to be better suited since the weakened muscles need not be cut unlike in open surgery. Proper choice of the type of repair is dependent on the size of the hernia and its contents, and this is crucial for a safe and long lasting repair. Use of anatomical and light weight meshes reduce long term postoperative pain. Newer techniques like eTEP ensure even larger hernias, which till recently needed open surgeries, can be treated laparoscopically.
Patients usually need one or two days of admission and can return to normal activity in a weeks’ time. However, it is advisable to avoid straining and lifting weights for 6 weeks following the surgery to ensure adequate time for healing.
 Removal of spleen (Splenectomy) is needed when spleen is needed in the following conditions.
Removal of spleen (Splenectomy) is needed when spleen is needed in the following conditions.
- Traumatic injury: when spleen is irreparably damaged due to trauma and causing intraabdominal bleeding.
- Primary splenic diseases: Serious diseases involving spleen like splenic abscesses ,cysts or tumors
- Hypersplenism: when due to certain conditions like ITP or portal hypertension, spleen is destroying normal blood cells leading to anemia or bleeding disorders.
In this surgery, spleen is safely separated from its attachments to the stomach and surrounding structures and removed. Laparoscopic splenectomy avoids a painful incision thus reducing pain and bleeding. This also helps in early recovery for the patients. Availability of vascular staplers and vessel sealing instruments helps in performing this procedure safely and minimal blood loss.
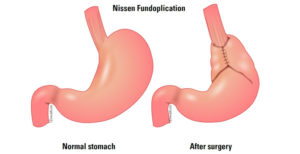 This is the surgery performed to cure GERD, also called as gastroesophageal reflux disease. Though GERD is quite common and majority of patients are treated with medication, surgery is advised in
This is the surgery performed to cure GERD, also called as gastroesophageal reflux disease. Though GERD is quite common and majority of patients are treated with medication, surgery is advised in
- Younger patients with GERD who otherwise need daily medications for the rest of life.
- patients with severe reflux esophagitis thus reducing the risk of complications like narrowing of esophagus (stricture) and tumors.
- Patients developing complications from GERD like Barretts’ esophagus which may lead to esophageal cancer.
The key steps of the procedure include
- Correcting the hiatus hernia which is the main cause for the reflux
- Tightening the weakened gastroesophageal valve
- Adequate fundal wrap; either complete (Nissen’s) or partial (Toupet/ Dor)
Patients usually need one day of hospital stay and can resume normal diet and activity from the next day. More than 99% of patients have improvement in their condition and stop medication altogether.
 Laparoscopic liver resections are increasingly offered to patients due to advances in the equipment and technical skill. Theses are usually offered to patients with
Laparoscopic liver resections are increasingly offered to patients due to advances in the equipment and technical skill. Theses are usually offered to patients with
- Certain cysts like hydatid cyst or cystadenomas
- Smaller peripherally located tumors of liver
The key principles for these procedures include
- Accurate preoperative planning of the resection by studying the internal anatomy of the liver. This is done by a CECT abdomen or a contrast enhanced MRI. This is essential to safely preserve the residual liver and its vital structures like blood vessels and bile ducts for a safe and fast recovery
- Tissue dissectors like CUSA, hydrojet or RFA for safely dividing the liver
- Vessel sealing devices like Ligasure and harmonic scalpel for control of bleeding.
Complicated liver abscesses like ruptured or multiple abscesses for which percutaneous procedures are not feasible can be treated with laparoscopic drainage.