GI Emergencies
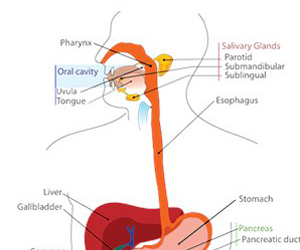 These are the acute conditions of the GI tract which have a sudden onset of symptoms with rapid progression and warrant immediate care for safe recovery. These need round the clock availability of experienced surgeons and supportive care for optimal results. The aim in these conditions will be safety, functional preservation and faster recovery in that order. In some conditions, better imaging modalities, supportive care and laparoscopy are helping in avoiding the need for surgery altogether or at least reducing the morbidity associated with it.
These are the acute conditions of the GI tract which have a sudden onset of symptoms with rapid progression and warrant immediate care for safe recovery. These need round the clock availability of experienced surgeons and supportive care for optimal results. The aim in these conditions will be safety, functional preservation and faster recovery in that order. In some conditions, better imaging modalities, supportive care and laparoscopy are helping in avoiding the need for surgery altogether or at least reducing the morbidity associated with it.
Factors which affect outcome in these conditions include
- Early approach for medical care
- Effective first aid and resuscitation
- Accurate and quick diagnosis
- Availability of trained and experienced gastroenterologists, surgeons and critical care specialists
Perforation
 This is a condition involving a breach in the gut wall leading to contamination of abdominal cavity and sepsis. Most common causes for perforation include
This is a condition involving a breach in the gut wall leading to contamination of abdominal cavity and sepsis. Most common causes for perforation include
- Duodenal ulcer perforation
- Typhoid perforation
- Appendicular perforation
- Perforation of small or large intestine due to obstruction/ tumours
Intestine is filed with bacteria and faecal material. Thease are prevented from entering blood stream by intestinal layers. Whenever intestine is ruptured these bacteria enter blood stream and cause serious sepsis. The main of treatment in these patients is to remove the cause for perforation (like inflammed appendix), prevent further contamination and adequate antibiotics for already existing sepsis.
Depending on the segment of intestine involved and the amount of contamination, either they are repaired or brought out as a stoma. In patients with early presentation, laparoscopic repairs are increasingly being offered for accelerated recovery.
Obstruction
 Intestinal obstruction is the condition when either small or large intestine is blocked. Intestine is essentially a tubular structure allowing passage of intestinal contents. Blockage of this passage prevents free passage of food and digestive juices which is essential for digestion. Obstruction of intestine leads to bloating of the abdomen and vomiting. This can present as a sudden event when there is a sudden complete obstruction or a gradual worsening of constipation in case of a progressive slow blockage.
Intestinal obstruction is the condition when either small or large intestine is blocked. Intestine is essentially a tubular structure allowing passage of intestinal contents. Blockage of this passage prevents free passage of food and digestive juices which is essential for digestion. Obstruction of intestine leads to bloating of the abdomen and vomiting. This can present as a sudden event when there is a sudden complete obstruction or a gradual worsening of constipation in case of a progressive slow blockage.
Most common causes for intestinal obstructions include
- Adhesions from previous surgeries: This is the most common cause. Normally intestines move freely in the abdominal cavity. Any infection or previous surgery causes adhesions when intestines are fixed to each other. This can lead to kinking or twisting of the intestine and obstruction. This can present even many years after previous surgeries.
- Hernia: these can be external hernias as previously described or sometimes rarely internal hernias.
- Tumors: Small and large intestinal tumors can present with either acute or slow onset obstruction. These are more common in older age groups.
The reasons for these are varied and need individualized treatment options. The main aim in these patients include removal of cause of obstruction (tumor/ hernia) and repair the damaged intestine. Laparoscopic surgeries are more useful in obstruction due to adhesions since they can prevent recurrence of fresh adhesions by the surgery itself. Development of endoluminal stents can obviate the need of surgery altogether.
Hemorrhage
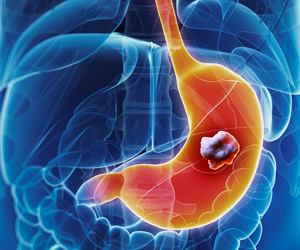
 Hemorrhage or bleeding can either be intraluminal which means bleeding into the gut or extra luminal in which case it can be from solid organs like liver or spleen. Depending on the severity of bleed, this can be a life threatening hemorrhage as seen following road traffic accidents or a slow ongoing bleed from a cancer of the intestine.
Hemorrhage or bleeding can either be intraluminal which means bleeding into the gut or extra luminal in which case it can be from solid organs like liver or spleen. Depending on the severity of bleed, this can be a life threatening hemorrhage as seen following road traffic accidents or a slow ongoing bleed from a cancer of the intestine.
Most common causes for intraluminal bleeding include ulcers, esophageal varices and tumors. The main principle in treating them include quick diagnosis and control of bleeding vessel by endoscopy and adequate resuscitation.
Extraluminal bleeding involves bleeding outside the intestinal tract, hence endoscopic methods are not possible for control of bleeding. Main causes for these include trauma leading to injury to liver, spleen or kidneys, and spontaneous rupture of abdominal tumors. Accurate diagnosis can be achieved by CT scan. Control of these bleeds can be done either by emergency surgery or angioembolization in selected cases. Modern procoagulant medicines, monitoring methods and interventional radiology can help in avoiding the need for surgery in some patients. Those patients who have severe bleeding need emergency surgery and good perioperative care for safe recovery.
Pancreatitis
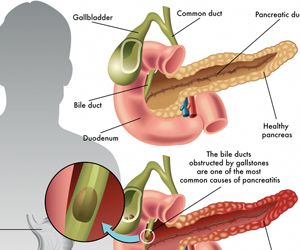 Uncontrolled abnormal activation of pancreatic digestive enzymes outside the intestinal tract leads to this condition. Most common causes for pancreatitis include
Uncontrolled abnormal activation of pancreatic digestive enzymes outside the intestinal tract leads to this condition. Most common causes for pancreatitis include
- Alcohol
- Gallstones
- Herreditary/ genetic causes
- Rare conditions like hypercalcemia and high triglycerides
Patients usually present with excruciating pain and severe metabolic abnormalities. Some patients who have severe pancreatitis present with features of sepsis, kidney/ respiratory failure. Initial management needs intensive ICU care aimed at correcting the abnormalities and preventing further complications. Following resuscitation and stabilisation, attention is directed at correcting the cause for pancreatitis (like gallstones) and assessing the severity of pancreatitis usually by CT scan. Role of surgery comes to treat septic complications by removing devitalized infected tissue (necrosectomy) or drainage of infected fluids (abscess). In view of friable tissues due to severe inflammation and brittle condition of patients, these procedures are challenging to surgeons and critical care specialists alike.