GI Emergencies
 These are the acute conditions of the GI tract which have a sudden onset of symptoms with rapid progression and warrant immediate care for safe recovery. The problems faced in these conditions include
These are the acute conditions of the GI tract which have a sudden onset of symptoms with rapid progression and warrant immediate care for safe recovery. The problems faced in these conditions include
Emergency surgery is designed to deal quickly with problems that can be life-threatening. It involves resuscitation and stabilization of the patient by a patient management team, preparing the patient for surgery, and post-operative and recovery procedures.
- Patient’s condition is often unstable, like low blood pressure and oxygen levels in the blood
- Limited time available for resuscitation
- Disease condition causing the emergency is severe, like ruptured gall bladder or appendix complicating the treatment.
In view of above conditions, round the clock availability of experienced surgeons and supportive care are essential for optimal results. The aim of treatment in these conditions will be safety, functional preservation and faster recovery in that order. Previously all these patients needed an open surgery as the only option, thus increasing the stress on these already fragile patients. Advances in supportive care and laparoscopy and interventional radiology enabled us to offer minimally invasive procedures in these patients for a safer and faster recovery.
 This is a condition involving a breach in the gut wall leading to contamination of abdominal cavity and sepsis. This can either be a duodenal ulcer perforation or a typhoid perforation or appendicular perforation. Depending on the segment of intestine involved and the amount of contamination, either they are repaired or brought out as a stoma. All these patients initially needed an open surgery which resulted in wound infections and secondary complications like abdominal wall dehiscence. Now majority of these patients can be managed laparoscopically for faster recovery. The surgeries include
This is a condition involving a breach in the gut wall leading to contamination of abdominal cavity and sepsis. This can either be a duodenal ulcer perforation or a typhoid perforation or appendicular perforation. Depending on the segment of intestine involved and the amount of contamination, either they are repaired or brought out as a stoma. All these patients initially needed an open surgery which resulted in wound infections and secondary complications like abdominal wall dehiscence. Now majority of these patients can be managed laparoscopically for faster recovery. The surgeries include
- laparoscopic appendicectomy for appendicular perforation
- laparoscopic cholecystectomy for ruptured gallbladder
- laparoscopic omental patch closure for duodenal/ gastric ulcer perforation
- laparoscopic colectomy for colonic perforation.
Recently, covered stents are being placed endoscopically to patch the perforations in patients diagnosed early thus avoiding surgery altogether.
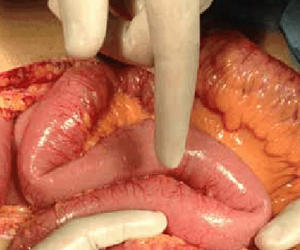
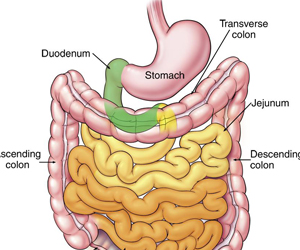 Gut being essentially a tubular structure allowing passage of intestinal contents. The reasons for these are varied and need individualized treatment options. These patients needed an open operation for recovery. Laparoscopy usually was avoided in view of unstable nature of patients and technical difficulty in handling the swollen and friable intestines. However, with advances laparoscopy is increasingly offered in the following conditions
Gut being essentially a tubular structure allowing passage of intestinal contents. The reasons for these are varied and need individualized treatment options. These patients needed an open operation for recovery. Laparoscopy usually was avoided in view of unstable nature of patients and technical difficulty in handling the swollen and friable intestines. However, with advances laparoscopy is increasingly offered in the following conditions
Adhesive obstruction: The most common cause for intestinal obstruction in recent times include adhesions from previous surgeries. Laparoscopy adhesiolysis has the advantage in that further adhesions are less frequent.
Obstructed Hernia: Hernia originate due to muscle weakness. Laparoscopic hernia repair ensures that the already weakened muscles are not cut as in open surgery.
Development of endoluminal stents can obviate the need of surgery altogether in patients who advanced tumors causing obstruction.
 Hemorrhage or bleeding can either be intraluminal which means bleeding into the gut or extra luminal in which case it can be from solid organs like liver or spleen. These patients, who have severe bleeding need emergency surgery and good perioperative care for safe recovery. Abdominal trauma is increasingly becoming common due to road traffic accidents. All these patients were previously offered exploratory laparotomy as alife safing measure. Recent advances include
Hemorrhage or bleeding can either be intraluminal which means bleeding into the gut or extra luminal in which case it can be from solid organs like liver or spleen. These patients, who have severe bleeding need emergency surgery and good perioperative care for safe recovery. Abdominal trauma is increasingly becoming common due to road traffic accidents. All these patients were previously offered exploratory laparotomy as alife safing measure. Recent advances include
- Multislice CT and supportive care: This helps in patients with mild bleeding. These patients can be safely monitored on medications with serial scans assessing for recovery. Surgery can altogether be avoided in these patients.
- Interventional Radiology: Angioembolization of bleeding intrabdominal vessels can be performed to stop the bleeding, This is especially useful in patients with pelvic fractures.
- Laparoscopic hemostasis/ repair: patients with liver/ splenic injury can now be treated with laparoscopy for control of bleeding.
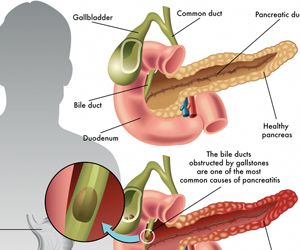 Uncontrolled abnormal activation of pancreatic digestive enzymes outside the intestinal tract can lead to this condition. Patients present with excruciating pain and severe metabolic abnormalities. Initial management needs intensive ICU care aimed at correcting the metabolic abnormalities and preventing further infective complications. Role of surgery comes to treat septic complications by removing devitalized infected tissue (necrosectomy) or drainage of infected fluids (abscess). Theses patients needed open necrosectomy and abscess drainage previously, which used to occasionally worsen the patient due to the added stress of surgery. Recently minimal access necrosectomy is being offered which reduce both the surgical stress in these patients and also avoid wound related complications. These can be
Uncontrolled abnormal activation of pancreatic digestive enzymes outside the intestinal tract can lead to this condition. Patients present with excruciating pain and severe metabolic abnormalities. Initial management needs intensive ICU care aimed at correcting the metabolic abnormalities and preventing further infective complications. Role of surgery comes to treat septic complications by removing devitalized infected tissue (necrosectomy) or drainage of infected fluids (abscess). Theses patients needed open necrosectomy and abscess drainage previously, which used to occasionally worsen the patient due to the added stress of surgery. Recently minimal access necrosectomy is being offered which reduce both the surgical stress in these patients and also avoid wound related complications. These can be
- Laparoscopic necrosectomy: through small ports placed into abdominal cavity
- Retroperitoneoscopic necrosectomy: here entry into abdominal cavity is entirely avoided by directly reaching the pancreas through the flank
- Transgastric endoscopic necrosectomy: Here surgery is altogether avoided by removing devitalised tissues through endoscopy